Rocky Mountain spotted fever (RMSF) is caused by the bacterium Rickettsia rickettsii. RMSF is characterized by a sudden onset of moderate to high fever (which can last for 2-3 weeks), severe headache, fatigue, deep muscle pain, chills and rash, which begins on the legs/feet or arms/hands, and may spread rapidly to the rest of the body. Symptoms usually appear within 2 weeks of the bite of an infected tick.
CDC Rocky Mountain spotted fever Information
Tularemia is caused by the bacterium Francisella tularensis. One way to become infected is through the bite of an infected tick. Symptoms of tularemia include swollen lymph glands and a skin ulcer at the site of the bite.
CDC Tularemia Information
Invasive Tick Species
Two additional tick species that are being monitored in Suffolk County are the Gulf Coast tick (Amblyomma maculatum) and the Asian longhorned tick (Haemaphysalis longicornis). Public health impacts are still being evaluated.
Diagnosis and Treatment
Be sure to seek medical attention if you become ill after a tick bite. Generally, an evaluation of symptoms and blood tests will be used in making a diagnosis. Most tick-borne disease patients respond well to appropriate antibiotic therapy. Prompt diagnosis and treatment improves outcome. Your physician will choose the medicine that is best for you.
Back to top of LIST
Personal Protection against Tick-Borne Diseases
Ticks will remain active year-round (when temperatures are above 40°F/4.4°C). Preventive measures should be used whenever tick-exposure is likely. Here are some steps to follow:
- Wear light-colored clothing
- Wear long pants and sleeves
- Tuck your pants into your socks
- Tuck your shirt into your pants
- Consider using repellents as directed
- Walk along the center of trails
- Conduct frequent clothing checks
- Once home, dry clothing on the highest temperature setting for 10 minutes to kill any ticks
- Carefully inspect your body for ticks
- Keep pets from tick infested areas and check them before entering the house.
Repellents
Repellents may be used to repel ticks and prevent tick attachment.
Tick Removal
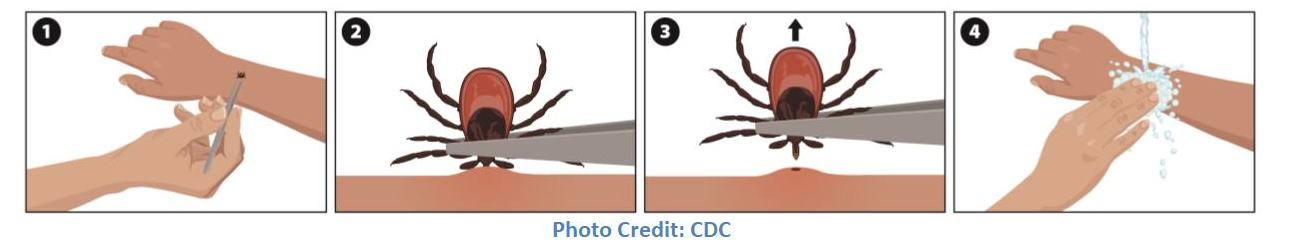
Studies have shown that the tick must stay on the body for 36 hours to transmit Lyme disease. Prompt and proper tick removal is essential and may decrease your chances of getting tick-borne diseases. The steps are:
- Use fine-point tweezers or tick-removal tools. Grasp the tick where its mouthparts enter the skin and pull the tick straight out.
- Do not twist or squeeze the tick’s body. Be patient – proper tick removal takes time.
- Do not use petroleum jelly, gasoline, lit matches, oils, or any other remedies to remove ticks. These methods may actually increase your chances of contracting a disease.
- After removing the tick, disinfect the bite area and wash your hands.
- Monitor the bite area for early signs and symptoms of Lyme disease
- Call your physician if you get any symptoms.
Ticks do not burrow under the skin, and any remaining mouthparts after tick removal will not transmit disease. However, additional aggravation of the bite site may cause secondary bacterial skin infections.
CDC Tick Bite: What to Do
Tick Management Suggestions for Homeowners
Ticks do not jump, fly, or fall from trees. They crawl close to the ground on leaves, brush and tall grass. Homeowners should consider:
- Keep lawn mowed and bushes trimmed;
- Remove lawn debris and leaf litter;
- Discourage rodents by reducing nesting sites (e.g. wood piles or holes in stone walls) or food sources (e.g. bird seed);
- Move lawn furniture and children’s toys away from wooded areas or wooded edges of your yard where ticks are more likely to be found.
Additional information regarding tick management: Tick Management Handbook by Kirby C. Stafford III, PhD (PDF file)
Back to top of LIST
Research, Management & Resources in Suffolk County
In 2011, Suffolk County established a Tick and Vector-Borne Diseases Task Force, which issued its final report in December 2015. The major recommendations of the Tick and Vector-Borne Diseases Task Force Final Report were: 1) survey Suffolk County tick populations in order to evaluate tick density and population ranges and 2) create a countywide tick-borne pathogen surveillance program to better understand pathogens present in tick populations and the related public health risk to county residents. In 2016, Suffolk County established the Tick Control Advisory Committee to provide Vector Control with recommendations to reduce tick-borne illness in the County for their Annual Plan of Work. Meeting minutes and committee recommendations can be found here. The committee has guided Suffolk County tick surveillance and control efforts by Department of Health’s Arthropod-Borne Disease Laboratory (ABDL) and Department of Public Works’ Division of Vector Control. Information on the Department of Public Works’ Division of Vector Control tick research and control efforts can be found on the Vector Control Website.
The following activities are underway:
Surveillance
- The Department of Health Services and the Department of Public Works are conducting tick surveillance in all 10 of Long Island's towns in order to study pathogens present in tick populations and the related public health risk to county residents.
- The Department of Public Works (DPW) is conducting surveillance at four locations year round to evaluate tick density and population ranges.
- Suffolk County's Tick Pathogen Surveillance Program
Tick Management for Municipalities and Commercial Pesticide Applicators
Suffolk County’s Division of Vector Control is conducting field trials using selected pesticides used by commercial applicators to test efficacy against ticks. Trials have been completed for some of the products. Municipalities, commercial pesticide applicators and other entities that are conducting tick control, may contact Suffolk County DPW Division of Vector Control for advice on best practices in Integrated Pest Management. Contact: 631-852-4270.
If you want a tick identified by photo, or have any questions about ticks or tick-borne diseases in Suffolk County, send them to:
Tick.Prevention@suffolkcountyny.gov
For identification purposes, please take well-lit, in-focus photographs of both the top and underside of the tick in question with a coin/ruler present to determine size.
We will reach out with a response as soon as we can.
Back to top of LIST